Opioid Crisis Resources
In 2018, the EHR Association launched its Opioid Crisis Task Force to examine how to best utilize electronic health record systems' data and capabilities as a tool in nationwide efforts to fight opioid abuse. Volunteer participants from member companies include pharmacists, doctors, nurses, and technical experts who are all focused on the unique contributions that EHRs have to offer federal and state policymakers, public health officials, and providers in the this of the opioid crisis. The Task Force has developed the following resources and tools which are freely available to all stakeholders.
EHRA's Opioid Crisis Task Force will continue to evaluate, add, and update these resources for furture use. If you have suggestions, questions, or recommendations, please contact knicholoff@ehra.org.
EHRA Opioid Tapering Implementation Guide for EHRs
The HIMSS Electronic Health Record Association (EHRA) is committed to bringing together leaders from our EHR developer community to collaborate on identifying viable solutions to industry challenges. In 2018, the Association’s Opioid Crisis Task Force was formed to research and provide recommendations on ways EHR technology can address the complex opioid crisis puzzle. One area researched extensively by the task force is clinical practice guidelines that can be operationalized to improve opioid stewardship and opioid tapering in clinical practice. This includes clinical recommendations from the United States CDC, VA/DOD, and HHS.
In January 2022, the EHRA published an Opioid Tapering Implementation Guide for Electronic Health Records. The goal is to enable an organization’s healthcare information technology (IT) team to more rapidly implement these best practices using EHR-based CDS tools. In addition, the EHR developer community can use this guide to steer the future development of new or updated products and services that can help hospitals, physician practices and other care environments implement these and other best practices.
Download the Opioid Tapering Implementation Guide.
Essential Components of an Opioid Tapering Plan Facilitated by an Electronic Health Record
State by State Landscape - EPCS & PDMP Tools
To evaluate the current status of how electronic prescribing of controlled substances (EPCS) and prescription drug monitoring program (PDMP) technologies are being utilized in the fight against prescription medication misuse, EHRA volunteers created a state by state landscape. Integration of these important tools within the EHR is critical to ensuring clinicians are able to easily access the data and tools they need at the point of care. Variation in the implementation and use of PDMPs and EPCS at the state level has created a barrier for the effective use of EHRs and other health information and technology in the fight against the opioid epidemic.
Download State by State Landscape.
EPCS Landscape: includes data on whether and when EPCS use is mandeted.
PDMP Landscape: includes detailed data on what, when, and by whom prescription data must be reported to the respective state's PDMP. Also, includes regulatory requirments, and information regarding interstate sharing of PDMP data and whether EHR integration is supported.
For key highlights on the problems and recommended solutions EHRA has identified within the state landscape, download our infographic.
CDC Opioid Guideline - Implementation Guide for EHRs
Initial research and conversations with providers focused on the question, "what do providers need from technology to support their efforts in the opioid crisis?" The input EHRA received led to the development of a guide to assist healthcare organization in implementing clinical practice guidelines within the EHR to improve opioid stewardship in clinical practice. Although the CDC Guideline is open cited by care Professionals who treat pain, it is seldom and inconsistently utilized in clinical practice.
One reason often cited to explain low adherence to clinical practice guidelines, the the CDC Guideline, is the lack of clinical decision support (CDS) tools within a provider's EHR workflow. While implementing CDS tools into an EHR can take many forms, the urgency of the opioid crisis spurred EHRA volunteers to take action to develop an EHR implementation guide that would provide organizations with "low lift" opportunities to operationalize each of the CDC's 12 guidelines in the best way.
Download the Implementation Guide.
Recommended Ideal Minimum Dataset for PDMP Response to EHR Inquiry
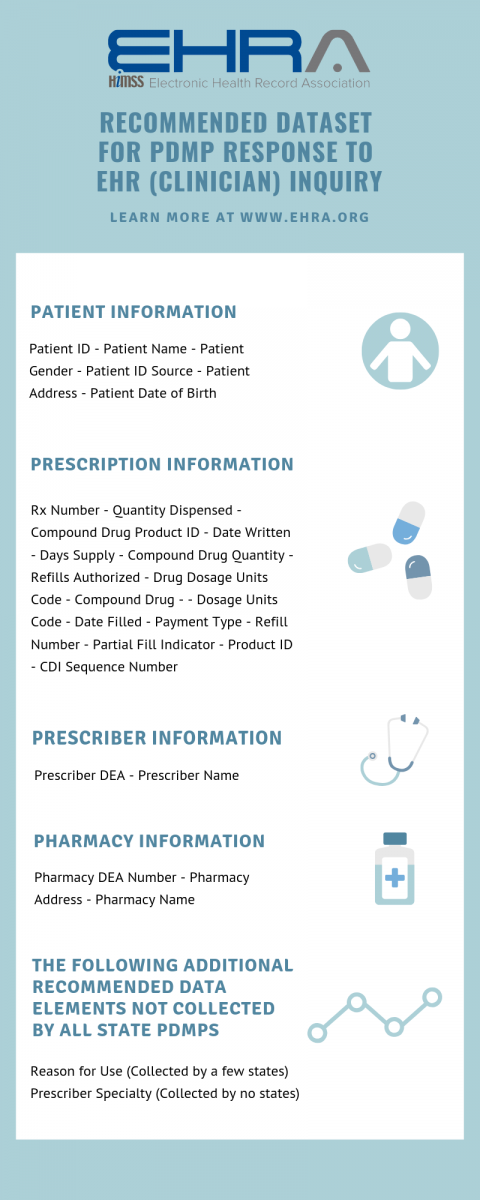 To address the lack of standardization for PDMP information available with the EHR, the Opioid Crisis Task Force developed an ideal minimum dataset to meet the needs of clinicians at the point of care. The dataset was developed with the assistance of numerous physicians and other healthcare professionals who helped refine the information to the minimal data necessary to have the most impact on clinical decision making.
To address the lack of standardization for PDMP information available with the EHR, the Opioid Crisis Task Force developed an ideal minimum dataset to meet the needs of clinicians at the point of care. The dataset was developed with the assistance of numerous physicians and other healthcare professionals who helped refine the information to the minimal data necessary to have the most impact on clinical decision making.
EHRA members recognize that the dataset itself is not the only critial factor in maximizing the value of the EHR/PDMP connection. Members strongly believe interoperability is a critical tool for improving seamless data exchange. The Task Force's next steps are to work with federal and state agencies to identify the necessary standards to acheive meaningful interoperability between the EHR and PDMP.
EHRA & ECRI Institute's Safe Practice Recommendations for Safer Opioid Prescribing
EHRA members together with the ECRI Institutes’ Partnership for Health IT Patient Safety have jointly published new guidance for safer opioid prescribing through electronic health records. The white paper, Safe Practice Recommendations for Safer Opioid Prescribing: Measures and Clinical Decision Support highlights the positive cycle of performance measurement and clinical decision support (CDS) incorporated into the EHR to enable safer opioid prescribing. Additionally, an accompanying implementation guide provides strategies that healthcare providers, across all care settings, can use not and with future innovation.
Publically available materials include:
- White Paper - Safe Practice Recommendations for Safer Opioid Prescribing: Measures and Clinical Decision Support
- Implementation Guide - Clinical Decision Support for Safer Opioid Prescibing: Recommedations and Implementation Strategies
- Literature Review - Measures and CDS for Safer Opioid Prescribing: A Literature Review
- Health IT Improves Opioid Prescribing Podcast - Episode jointly produced with EHRA and the Partnership for Health IT Safety looks at safe practice recommendations for opioid prescribing.
The EHRA-ECRI Joint Project on Safer Opioid Prescribing demonstrated the value of combining Patient Safety Organization (PSO) data gathering and analytics with developer expertise in a collaborative environment. The combined expertise of the EHRA members who participated on the workgroup and knowledge from the data analysis and evidence synthesis contributed to the overall recommendations and implementation strategies.


